Health
The Connection Between HCC Gaps and Reimbursement Losses: How to Close the Loop

A healthcare provider reviews year-end financial reports only to realize that reimbursements are significantly lower than expected. Despite delivering quality care, underreported risk scores have led to substantial revenue loss. The root cause? Unrecognized Hierarchical Condition Category (HCC) gaps.
HCC gaps occur when chronic conditions and comorbidities are not fully documented, resulting in inaccurate risk scores and reduced reimbursements. With updates from CMS HCC V24 to V28, the way risk adjustment factors (RAF) are calculated has evolved, making it even more critical for healthcare organizations to close documentation gaps. Without addressing these issues, providers risk losing substantial revenue while also exposing themselves to compliance risks.
Why HCC Gaps Lead to Reimbursement Losses
Incomplete Documentation Affects Risk Scores
When chronic conditions are underreported or missing from documentation, the patient’s risk adjustment factor (RAF) score is lower than it should be. Since reimbursements under Medicare Advantage and other risk-based payment models depend on these scores, incomplete documentation directly reduces revenue.
Missed Opportunities for Risk Capture
Many chronic conditions, such as diabetes with complications, COPD, and heart failure, impact a provider’s risk score. If these conditions are not captured at every encounter, the patient appears to be healthier than they actually are, leading to miscalculated reimbursements.
Increasing Compliance Scrutiny
CMS expects accurate and complete documentation to justify risk-adjusted payments. Incomplete coding can trigger audits, resulting in penalties, clawbacks, and reputational risks. Healthcare organizations that fail to address HCC gaps may face both financial and regulatory consequences.
Understanding the Impact of CMS HCC V24 to V28 Updates on Risk Adjustment
Changes in HCC Categories
With CMS HCC V24 to V28 updates, several HCC categories have been restructured, merged, or removed. These changes mean that coders and providers must adjust their documentation practices to align with the latest risk adjustment criteria.
New Documentation Requirements
Providers must capture conditions with more specificity to meet updated CMS standards. This shift demands real-time risk assessment and better coding accuracy.
Financial and Compliance Implications
Failure to adapt to CMS HCC V28 could lead to incorrect risk stratification, lower reimbursements, and increased audit risks. Healthcare organizations that do not proactively adjust coding practices may find themselves facing unexpected financial setbacks.
Key Strategies to Close HCC Gaps and Optimize Reimbursement
- Implement Real-Time Risk Adjustment Documentation
- Utilize AI-powered tools that prompt providers to document risk-adjusted conditions during patient encounters.
- Ensure complete and specific coding to avoid underreporting of chronic conditions.
- Embed coding guidance within electronic health records (EHRs) to streamline real-time documentation.
- Train Providers and Coding Teams on CMS HCC V24 to V28 Changes
- Offer ongoing education on how the updated model impacts coding requirements and financial outcomes.
- Encourage collaborative coding workflows between clinicians and documentation specialists to ensure accurate HCC capture.
- Provide regular coding audits and case-based training to reinforce best practices.
- Conduct Pre-Visit Risk Assessments
- Use predictive analytics to identify patients with potential undocumented HCC conditions before their appointments.
- Ensure risk scores accurately reflect patient health complexity at the point of care by reviewing past medical histories and previously documented diagnoses.
- Utilize AI-driven patient stratification tools to prioritize high-risk individuals for documentation review.
- Perform Routine Documentation Audits
- Regularly review clinical documentation to detect and correct missing HCC codes before claims submission.
- Prevent audit-triggering discrepancies by ensuring coding consistency across encounters and specialties.
- Implement CDI-led retrospective reviews to identify trends in underreported conditions.
- Integrate AI-Driven Risk Adjustment Solutions
- Automate the identification of HCC gaps using machine learning tools that analyze past and current documentation.
- Provide real-time feedback to providers, helping them capture missing conditions proactively.
- Reduce administrative burden by automating repetitive risk adjustment coding tasks.
Avoiding Common Pitfalls in Closing HCC Gaps
Assuming Past Coding Practices Are Still Valid
With CMS HCC V24 to V28 updates, relying on outdated coding approaches can lead to revenue loss. Providers must adjust documentation strategies to align with the latest risk adjustment framework.
Relying Solely on Retrospective Audits
Waiting until after claims submission to address documentation gaps means providers miss opportunities to correct risk scores in real time. A proactive approach, integrating concurrent coding, is more effective.
Neglecting Provider Engagement
If physicians don’t understand the financial and compliance risks associated with incomplete documentation, they may deprioritize HCC capture. Education, feedback loops, and real-time guidance are crucial to bridging this gap.
How Closing the HCC Gap Improves Financial and Patient Outcomes
Maximizes Reimbursement Potential
Proper risk capture ensures that providers are compensated fairly for the level of care provided. With optimized risk scores, organizations receive accurate and appropriate funding.
Reduces Audit Risks and Compliance Issues
Ensuring complete documentation aligns with CMS guidelines, minimizing financial penalties and reducing the likelihood of an audit-triggered reimbursement clawback.
Enhances Patient Care Planning
Accurate documentation allows for better coordination of care, ensuring patients receive the interventions they need. This is particularly critical for managing chronic diseases, where accurate coding directly impacts treatment plans.
Actionable Steps for Healthcare Organizations
Assess Current HCC Capture Rates
Analyze documentation trends to identify where risk scores are being underreported. Compare past coding patterns to current CMS guidelines to detect gaps.
Upgrade Risk Adjustment Technology
Ensure EHR systems support AI-driven HCC detection and real-time coding feedback. Risk adjustment software should be capable of integrating into daily workflows to enhance efficiency.
Monitor Reimbursement Trends
Track whether RAF scores and financial performance improve as HCC documentation becomes more accurate. Identify areas where coding interventions lead to better revenue outcomes.
Engage Providers in CDI Initiatives
Encourage providers to see risk adjustment as a tool for enhancing both patient care and financial sustainability. Develop a culture of continuous learning and quality improvement.
Final Thoughts
HCC gaps represent a significant yet preventable source of reimbursement loss for healthcare providers. With the transition from CMS HCC V24 to V28, the need for accurate and complete documentation is more pressing than ever. By implementing AI-driven solutions, real-time documentation support, and proactive provider training, organizations can close the loop on HCC capture, ensuring compliance, financial sustainability, and high-quality patient care.
Closing HCC gaps is not just a financial strategy—it’s a commitment to more accurate patient risk stratification, better healthcare planning, and a stronger, more efficient revenue cycle. Healthcare providers who prioritize risk adjustment accuracy will be better positioned to thrive in an evolving regulatory and financial landscape.
For More Information Visit Loopermagazine
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Jordan Broad?: The Untold Story of Ashley Broad Husband
-
 Celebrity1 year ago
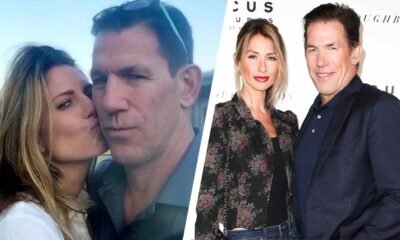
Celebrity1 year agoWho Is Mary Ryan Ravenel?: Inside The Life Of Thomas Ravenel’s Ex-Wife
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Noelle Inguagiato?: The Untold Story Of Jesse Watters Ex-Wife
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Dolphia Parker?: Everything About Dan Blocker’s Wife






